- Home
- About
- Editorial Team
- Browse
- Submissions
- Advertising
- ESMINT Website

The Journal of the Swiss Society of
Minimally Invasive Neurological Therapy
The Journal of the Swiss Society of
Minimally Invasive Neurological Therapy
Overlapping stents in "Y" configuration for anterior circulation aneurysms
EJMINT Original Article, 2013: 1304000095 (21st January 2013)
Abstract
Keywords: Y stent, cerebral aneurysm, embolisation, wide-neck aneurysm, stent-assisted coiling, anterior circulation aneurysm
Introduction
Endovascular options for treating intracranial aneurysms have rapidly evolved over the past two decades. Wide-neck cerebral aneurysms traditionally posed a significant barrier to endovascular repair [1]. Balloon remodeling, stent-assisted coiling techniques and flow diversion, however, have recently provided effective and safe endovascular treatment options for wide-neck aneurysms [1]. Wide-neck aneurysms that incorporate vascular bifurcations and involve both daughter vessels have proven difficult to safely treat with coil embolisation, balloon-assisted embolisation or single stent-assisted coiling due to the risk of coil prolapse and migration through the wide unprotected or incompletely protected aneurysm neck. Recently, however, the technique of dual stents placed in a “Y” configuration (Y-stenting) has been described as an endovascular strategy to treat wide-neck bifurcation aneurysms involving both daughter vessels. The Y-stenting technique for treatment of cerebral aneurysms was originally described in 2004 by various groups for basilar apex aneurysms [2-5] The application of this technique was expanded to anterior circulation aneurysms with the first description of Y-stenting of a middle cerebral artery (MCA) aneurysm [5]. Since these initial reports there have been a number of small case series that have reinforced the therapeutic efficacy of this technique in treating wide-necked bifurcation aneurysms. In 2011, Spiotta et al. reported mid-term results of patients treated with Y-stenting, including 18 basilar artery aneurysms and 1 anterior communicating artery (Acomm) aneurysm [6]. They report 26 % Raymond class 1, 26 % Raymond class 2 and 47 % Raymond class 3 initial outcomes; at mid-term follow-up they report 63 % Raymond class 1 angiographic outcome. To date, the majority of reported Y-stents have been used to treat basilar artery aneurysms [5-9]. In this paper we present the largest published experience with Y-stenting in the anterior circulation, including the first report of Y-stenting for treatment of 2 internal carotid artery (ICA) aneurysms (Table 1). We report our experience treating aneurysms with multiple stents in a Y-configuration for reconstruction of anterior circulation bifurcations.
Methods
After obtaining internal review board approval we performed a retrospective review of all patients undergoing Y-stenting of intracranial anterior circulation aneurysms at Rush University Medical Center. All cases were performed by the senior author (DKL). We reviewed our database, medical records, operative reports and radiological studies to provide data pertaining to the clinical presentation, surgical indications, aneurysm type, immediate and late surgical outcomes and complications.
Patient Selection
Patients with unruptured intracranial aneurysms greater than 5 mm in diameter were considered for treatment. Additional indications for patients with small aneurysms included history of aneurysmal subarachnoid haemorrhage (SAH), multiple intracranial aneurysms, systemic vasculopathy and aneurysmal growth on serial imaging. The Y-stent technique was not used as a primary reconstruction strategy; rather, it was used as a bailout strategy in cases where coiling or aneurysmal reconstruction was not feasible using conventional single-stent or balloon remodeling techniques. This technique was applied to a minority of patients (~3 %, 14/434) treated with stent-assisted embolisation for wide-neck anterior circulation aneurysms (Figs 1, 2) (Table 2).
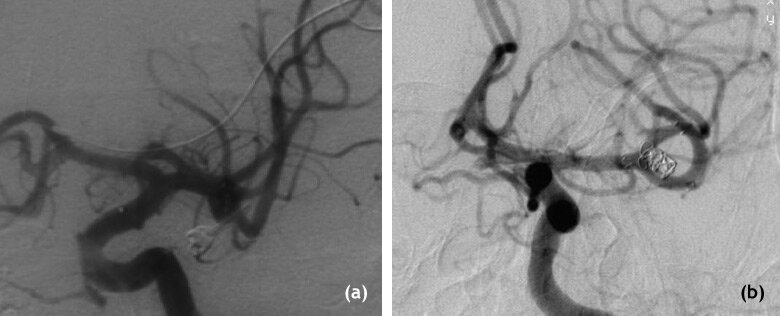 Figure 1(a) AP angiogram of recurrent wide-neck MCA aneurysm after microsurgical clipping in patient with prior subarachnoid hemorrhage. (b) AP angiogram at 1-year follow-up of same patient after Y-stent and coil reconstruction of the MCA bifurcation aneurysm with Raymond class 1 occlusion of the aneurysm.
Figure 1(a) AP angiogram of recurrent wide-neck MCA aneurysm after microsurgical clipping in patient with prior subarachnoid hemorrhage. (b) AP angiogram at 1-year follow-up of same patient after Y-stent and coil reconstruction of the MCA bifurcation aneurysm with Raymond class 1 occlusion of the aneurysm.
 Figure 2(a) Oblique angiogram of a wide-neck MCA bifurcation aneurysm prior to treatment in a patient with multiple intracranial aneurysms. (b) Initial attempts at aneurysmal reconstruction using the single-stent and coiling technique were not possible due to coil prolapse into the superior branch of the MCA bifurcation. (c) Intraoperative DynaCT after a second stent was placed in a Y-configuration, reconstructing the bifurcation and protecting the superior division of the MCA for coil embolization of the aneurysm. (d) Oblique angiogram after treatment with Y-stent and coiling technique demonstrating Raymond class 1 aneurysmal occlusion.
Figure 2(a) Oblique angiogram of a wide-neck MCA bifurcation aneurysm prior to treatment in a patient with multiple intracranial aneurysms. (b) Initial attempts at aneurysmal reconstruction using the single-stent and coiling technique were not possible due to coil prolapse into the superior branch of the MCA bifurcation. (c) Intraoperative DynaCT after a second stent was placed in a Y-configuration, reconstructing the bifurcation and protecting the superior division of the MCA for coil embolization of the aneurysm. (d) Oblique angiogram after treatment with Y-stent and coiling technique demonstrating Raymond class 1 aneurysmal occlusion.
Surgical Technique
All procedures were done under general anesthesia. A strict antiplatelet protocol was used: patients received aspirin (325 mg) and clopidogrel (75 mg) daily for 5 days or were loaded with 600 mg of clopidogrel and 325 mg of aspirin at least 2 hours prior to the procedure. At the beginning of each procedure, antiplatelet activity was measured using point-of-care aspirin and P2Y12 assays (VerifyNow, Accumetrics, San Diego, CA). In cases where anti-platelet therapy was not therapeutic – aspirin reaction unit above 550 or P2Y12 reaction unit below 250 or less than 30 % inhibition – an intra-arterial loading dose of 0.25 mg/kg abciximab (0.25 mg/kg), was given prior to stent placement, followed by a 12 h intravenous abciximab infusion (0.125 mcg/kg/min or 10 mcg/min). Abciximab was also given if thrombus developed inside of the stent or when patients had a new neurological deficit after treatment and a computerized tomography (CT) scan showed no intracerebral haemorrhage. Clopidogrel 600 mg was given after the procedure if P2Y12 reaction unit was below 250 or less than 30 % inhibition. Intraprocedural heparinization was utilized with a target activated clotting time of 250 to 300 s. The anticoagulation and antiplatelet regimens were consistent in every case.
The distal end of the first stent was placed in the larger of the two daughter vessels or into the daughter vessel that was most challenging to access with the microcatheter; the proximal end was deployed in the parent vessel. The second stent was navigated through the interstices of the first stent with its distal end placed in the smaller daughter vessel of the bifurcation and its proximal end in the parent artery, overlapping the first stent’s proximal end. After successful placement of the stents in a Y-configuration, a microcatheter was navigated into the aneurysm sac and coils were deployed until the aneurysm was obliterated. Post-procedurally all patients underwent non-contrast head CT. Patients were maintained on aspirin indefinitely and clopidogrel for 6 months post-procedurally. Follow-up angiography was obtained at 6 months and 12 months. A combination of Neuroform (Boston Scientific-Target, Fremont, CA), Neuroform EZ (Boston Scientific-Target, Fremont, CA) and Enterprise (Cordis Neurovascular, Miami, FL) stents were used to reconstruct the aneurysm neck. Matrix (Boston Scientific, Boston MA), Hydrocoil (MicroVention, Aliso Viejo, CA), Orbit (Cordis, Miami Lakes, FL) and GDC platinum (Boston Scientific, Boston, MA) coils were used to obliterate the aneurysm sac after Y-stent placement. One patient who had previous aneurysm clipping was treated with Y-stenting without coil embolisation.
Results
Between 2004 and 2011 we identified 14 patients who underwent Y-stenting of anterior circulation aneurysms. Of these, 10 patients underwent Y-stenting of MCA aneurysms, 2 patients underwent Y-stenting of ICA aneurysms and 2 patients underwent Y-stenting of Acomm aneurysms.
Middle Cerebral Artery Y-Stents
The average age of patients undergoing Y-stent reconstruction of MCA aneurysms was 54.7 years (range 33-67). 70 % (7/10) patients were female. The majority (7/10, 70 %) of MCA aneurysms were located on the right side, 40 % (4/10) of aneurysms were found incidentally and 40 % of patients (4/10) had multiple cerebral aneurysms. One patient underwent prior clipping of a MCA aneurysm that recurred on follow-up angiography, necessitating endovascular intervention. One patient’s aneurysm was followed with serial imaging and demonstrated interval change in aneurysm morphology. One patient had multiple prior intracranial aneurysms and the treated MCA aneurysm was discovered on surveillance angiography. One patient presented with left hemiparesis from an ischemic stroke related to thromboembolism from an intra-aneurysmal clot. One patient presented with acute SAH with right hemiplegia from a left sided MCA aneurysm and was found to have bilateral MCA aneurysms. A total of 30 % (3/10) of patients had aneurysms that were less than 10 mm in size and had necks less than 4 mm in size, 60 % (6/10) had aneurysms that were less than 10 mm in size, but had necks greater than 4 mm and 10 % (1/10) had aneurysms between 10 mm and 25 mm in size (Table 3).
Of the 10 patients with MCA aneurysms treated with Y-stenting, 40 % (4/10) had successful Raymond class 1 occlusion of the aneurysm (complete obliteration), 40 % (4/10) had Raymond class 2 occlusion (residual aneurysm neck) and 20 % (2/10) had Raymond class 3 occlusion (residual aneurysm sac) at the conclusion of the initial procedure. One patient had a groin haematoma that was complicated by a subsequent deep vein thrombosis, 1 patient had a femoral artery pseudoaneurysm and 1 patient experienced transient left arm weakness that resolved prior to discharge. The average length of hospitalization was 1.9 days (range 1-5).
60 % (6/10) of patients underwent follow-up angiography after Y-stenting of their MCA aneurysm. 100 % of patients who had follow-up angiography showed Raymond class 1 occlusion of the Y-stented MCA aneurysm. Three patients were initially Raymond class 1 and re-demonstrated Raymond class 1 aneurysmal occlusion on follow-up angiography. Two patients were initially Raymond class 2 and were found to have advanced to Raymond class 1 occlusion on follow-up. One patient was initially Raymond class 3 and advanced to Raymond class 1 on follow-up. None of the patients demonstrated coil compaction or in-stent stenosis on 6-month follow-up angiography, and none developed new neurological deficits after MCA Y-stenting. One patient had an isolated post-procedural transient ischemic attack (TIA), and 1 patient had recurrent TIAs after stopping clopidogrel; these episodes ceased with re-institution of clopidogrel. None of the patients suffered a SAH after Y-stenting of their MCA aneurysm. Average follow-up was 14.5 months (range 6-43) (Table 4).
Internal Carotid Artery Y-Stents
The average age of the 2 patients undergoing Y-stent reconstruction of ICA aneurysms was 60.5 years (range 44-77) and both were female. One aneurysm was found in a patient being evaluated for dizziness; the second was found in a patient who presented with a SAH. Both patients had multiple cerebral aneurysms, and both were neurologically intact prior to treatment.
One of the 2 Y-stented ICA aneurysms had initial Raymond class 1 occlusion. This same patient pre-operatively suffered from gastritis and had an intra-operative upper gastrointestinal bleed, necessitating early termination of the procedure. The patient had intraoperative somatosensory evoked potentials (SSEP) changes in the ipsilateral (left) hemisphere without angiographic evidence of vascular occlusion and awoke with a right-sided hemiparesis. Post-operative head CT was negative for intracranial haemorrhage. The patient continued to demonstrate post-operative haemodynamic instability and suffered multiple cardiac arrests and ultimately died on post-operative day 1. The other patient tolerated the procedure without complication and initially had Raymond class 3 occlusion of the aneurysm.
The second patient underwent follow-up angiography after Y-stenting of their ICA aneurysm. This patient showed Raymond class 1 occlusion of the Y-stented ICA aneurysm at 6-month follow-up angiography and did not demonstrate coil compaction or in-stent stenosis. There were no late complications from ICA Y-stent. Average follow-up was 6.5 months (Table 5).
Anterior Communicating Artery Y-Stents
The average age of the 2 patients undergoing Y-stent reconstruction of Acomm aneurysms was 57 years (range 56-58), and 1 was female. One aneurysm was found in a patient who presented with headaches and the other was found to be a recurrence of a previously clipped Acomm aneurysm that was identified on surveillance angiography. Neither patient harboured additional aneurysms, and both patients were neurologically intact prior to treatment.
One of the 2 Y-stented Acomm aneurysms had initial Raymond class 1 occlusion. The other patient who had previous unsuccessful microsurgical clipping only had stents placed (Enterprise and Neuroform) without coiling due to concern for perforators and had initial Raymond class 3 occlusion after the Y-stent only construct. On follow-up angiography neither patient had change in Raymond classification. Neither patient had any complication from the Y-stenting procedure. The patient with Raymond class 3 occlusion had 6 months of follow-up; the patient with Raymond class 1 occlusion had 59 months of follow-up (Table 6).
Discussion
We report the largest series to date on the application of Y-stenting to wide-neck anterior circulation bifurcation aneurysms. This series of 14 patients with an average follow-up of 14 months complements the existing literature describing the application of Y-stenting to complex intracranial aneurysms. Specifically, it demonstrates the technical feasibility and therapeutic efficacy of Y-stenting for wide-neck bifurcation aneurysms in the anterior circulation. Y-stenting has been shown to be a viable endovascular strategy in treating posterior circulation aneurysms [6]. This series provides similar data for the application of Y-stenting to anterior circulation aneurysms. The use of a Y-stent construct in our institution has been infrequent: ~3 % of wide-neck aneurysms and 0.7 % of all aneurysms treated during the study period were treated with a Y-stent construct. Though necessary in a minority of patients, we have found the use of this technique to be a valuable tool in the endovascular treatment of these complex aneurysms. It has enabled coil embolisation in cases that otherwise would have been unable to be adequately or safely treated endovascularly. It has also enabled the application of a greater coil density to the aneurysm neck, which predictably improved both the tendency for progressive aneurysmal thrombosis and the durability of the repair.
Single stent-assisted coiling in wide-necked bifurcation aneurysms fails to reconstruct the residual neck of the aneurysm that involves the unstented daughter vessel. Similarly, flow diverters only address the portion of the aneurysmal neck of the stented daughter vessel and the safety of this technique in protecting perforating vessels and branches is unproven. Double-balloon remodeling technique offers a potential alternative to stent reconstruction of vascular bifurcations; however, there remains a concern that the durability of this technique may be inferior to stent-assisted techniques. Newer devices such as intrasacular flow disrupters have also been described in the treatment of bifurcation aneurysms [10]. Only early follow-up is available, however, and intrasacular flow disrupters may still be susceptible to migration when applied to wide-necked bifurcation aneurysms. Open surgical alternatives for this category of aneurysms are craniotomy with either microsurgical clipping or aneurysmal trapping and bypass. A final management alternative for these difficult aneurysms is observation.
In this series, aneurysmal reconstruction using a Y-stent technique has yielded durable results, at least in the mid-term follow-up. The MCA bifurcation is the most common location where a Y-stent construct was employed in the anterior circulation. We found excellent results in the cohort of MCA aneurysms, all of which achieved Raymond Class 1 occlusion without any permanent complications. There were 2 access related complications and 1 transient neurologic complication in this cohort of Y-stented wide-necked MCA bifurcation aneurysms.
The results in the MCA group compare favourably to our results in the Acomm and ICA groups. In the ICA group, 1 of the 2 patients died. While this mortality was attributable to a systemic complication (GI bleed and subsequent cardiac arrest), the patient also suffered an observable hemiparesis indicative of a concomitant neurological injury. Moreover, the fatal complication was almost certainly related to the peri-procedural antithrombotic therapy. In the Acomm group, 1 patient who had previously failed clipping underwent Y-stenting of the aneurysm. Coils were unable to be placed due to concern for perforators originating from the dome of the aneurysm. This achieved a suboptimal technical outcome with initial and follow-up Raymond class 3 occlusion. Overall, in the non-MCA group (ICA and Acomm combined) we found 2/4 (50 %) with Raymond class 1 outcomes, 1/4 (25 %) Raymond class 3 outcome and 1/4 (25 %) mortality. The apparent clustering of suboptimal and poor outcomes in the non-MCA group may be informative. Y-stent placement is limited by the requirement for adequate luminal caliber of the daughter vessels for stent placement. Anatomically, the non-MCA sites are more likely to contain daughter vessels that are relatively smaller than their parent vessels, while the MCA bifurcation is more likely to contain comparably sized parent and daughter vessels. These complications highlight the importance of careful patient selection, both from a technical and systemic perspective, in treating complex intracranial aneuryms. Important considerations include careful evaluation of systemic contraindications to antithrombotic therapy, review of parent and daughter vessel caliber and assessment of perforators emanating from the aneurysm.
Additionally, the evolution of aneurysmal filling over time after Y-stent reconstruction may be instructive. We observed that 83 % (5/6) of patients who initially were Raymond class 2 or 3 progressed to Raymond class 1 occlusion at follow-up angiography. We take this high rate of delayed aneurysmal occlusion to be evidence of aneurysmal thrombosis related to altered intrasaccular haemodynamics caused by placement of the Y-stent. Similar evolution of intrasaccular thrombosis has been noted with the use of flow diverting stents [11]. The specific haemodynamic alterations caused by Y-stent constructs both in the aneurysmal sac and in the vessel lumen deserve further study.
Two patients in this series presented with aneurysmal SAH. Both were treated successfully and without complication using Y-stenting in the acute phase of SAH. The application of stenting in ruptured aneurysms deserves further investigation.
Y-stenting techniques have enabled successful endovascular reconstruction of complex wide-neck bifurcation aneurysms that would otherwise have not been treatable with this therapeutic modality. However, there are a number of concerns specific to this endovascular approach that demand further study. Specifically, the application of dual stents requires increased vascular manipulations and theoretically exposes the patient to increased risks of intraoperative vessel damage compared to coiling or single-stent assisted coiling. This risk may be more pronounced in cases of acutely ruptured aneurysms. As with other stenting techniques, its application remains confined by the diameter of the daughter vessels, as they both must be an adequate diameter to accept the distal end of a stent. Moreover, there is increased theoretical risk of impaired construct endothelialisation with the overlapping stents and luminal struts that are inherent to Y-stent constructs. This may predispose Y-stent constructs to a higher risk of thromboembolic complications and in-stent stenosis. In our series and in previous series [6] the incidence of in-stent stenosis and delayed symptomatic thromboembolic complications has been minimal. The long-term patency, however, remains to be defined for Y-stents. Similarly, the optimal anti-platelet regimen has not yet been established for these constructs.
Y-stents offer an alternative treatment strategy to reconstruct complex wide-neck bifurcation aneurysms previously not amenable to endovascular therapy. This series demonstrates the application of this technique to a series of patients with anterior circulation aneurysms. We observed favourable results in the larger MCA group and more varied outcomes, including 1 peri-procedural mortality, in the ICA and Acomm group. We await long-term follow-up of this initial cohort of patients treated with Y-stents to define rates of in-stent stenosis, aneurysmal recurrence rates and aneurysmal rupture. Further studies comparing the efficacy and risks of Y-stenting techniques to dual-ballon remodeling, intrasacular flow disrupters, microsurgical clipping and observation are needed to define the optimal treatment of wide-neck bifurcation aneurysms.
Conflict of interest
We declare that we have no conflict of interest.
References
- Lanzino G, Kanaan Y, Perrini P, Dayoub H, Fraser K; Emerging concepts in the treatment of intracranial aneurysms: stents, coated coils, and liquid embolic agents; Neurosurgery 2005;57:449-59; discussion -59.
- Chow MM, Woo HH, Masaryk TJ, Rasmussen PA; A novel endovascular treatment of a wide-necked basilar apex aneurysm by using a Y-configuration, double-stent technique; AJNR Am J Neuroradiol 2004;25:509-12.
- Akpek S, Morsi H, Benndorf G, Strother CM, Mawad ME; Reconstruction of the basilar tip with T stent configuration for treatment of a wide-neck aneurysm; J Vasc Interv Radiol 2004;15:1024-6.
- Perez-Arjona E, Fessler RD; Basilar artery to bilateral posterior cerebral artery 'Y stenting' for endovascular reconstruction of wide-necked basilar apex aneurysms: report of three cases; Neurol Res 2004;26:276-81. [PubMed]
- Sani S, Lopes DK; Treatment of a middle cerebral artery bifurcation aneurysm using a double neuroform stent "Y" configuration and coil embolizationembolisation: technical case report; Neurosurgery 2005;57:E209; discussion E.
- Spiotta AM, Gupta R, Fiorella D, et al.; Mid-term results of endovascular coiling of wide-necked aneurysms using double stents in a Y configuration; Neurosurgery 2011;69:421-9.
- Cekirge HS, Yavuz K, Geyik S, Saatci I; A novel "Y" stent flow diversion technique for the endovascular treatment of bifurcation aneurysms without endosaccular coiling; AJNR Am J Neuroradiol 2011;32:1262-8. [PubMed]
- Lozen A, Manjila S, Rhiew R, Fessler R; Y-stent-assisted coil embolizationembolisation for the management of unruptured cerebral aneurysms: report of six cases; Acta Neurochirurgica 2009;151:1663-72. [PubMed]
- Darkhabani ZM, Lazzaro MA, Zaidat OO; Pericallosal artery aneurysm treatment using Y-configuration stent-assisted coil embolizationembolisation: a report of four cases; J Neurointerv Surg 2012.
- Pierot L, Liebig T, Sychra V, et al.; Intrasaccular Flow-Disruption Treatment of Intracranial Aneurysms: Preliminary Results of a Multicenter Clinical Study; American Journal of Neuroradiology 2012;33:1232-8.
- Fischer S, Vajda Z, Aguilar Perez M, et al.; Pipeline embolizationembolisation device (PED) for neurovascular reconstruction: initial experience in the treatment of 101 intracranial aneurysms and dissections; Neuroradiology 2012;54:369-82. [PubMed]
Copyright © 2013 Swiss association of Minimally Invasive Neurological Therapy
Swiss association of Minimally Invasive Neurological Therapy Alerts
 latest news & articles
latest news & articles
Keywords
- intracranial aneurysms
- endovascular treatment
- flow diverter
- clopidogrel resistance
- training
- UEMS
- charter
- neuroradiology
- Interventional
- INR
- pharmacogenetics
- aneurysm
- pipeline embolisation device
- silk flow diversion device
- stents
- intracranial
- stroke
- interventional neuroradiology
- thrombectomy
- thrombolysis
- endovascular
- stroke treatment
- mechanical thrombectomy
- stent retriever
- magnetic resonance angiography
- intracranial aneurysm
- subarachnoid haemorrhage
- computed tomography
- angiography
- flow diversion
- cerebral
- delayed rupture
- Y stent
- cerebral aneurysm
- embolisation
- wide-neck aneurysm
- stent-assisted coiling
- anterior circulation aneurysm
- acute ischemic stroke
- randomised clinical trials
- carotid artery stenting
- high-risk
- complications
- flow disruption
- WEB
- tPA
- stent
- balloon-assisted
- stability
- sedation
- anesthesia
- transcarotid
- platelets
- haemorrhage
- thrombosis
- carotid stenting
- proximal balloon protection
- intracranial haemorrhage
- coils
- clipping
- acute stroke therapy
- ischaemic stroke
- MRI
- rtPA
- cranial venous outflow obstruction
- jugular venoplasty
- chronic fatigue syndrome
- idiopathic intracranial hypertension
- lumbar puncture
- cerebrovascular occlusion
- brain infarction - posterior circulation
- brain infarction – anterior circulation
- predictors
- femoral arterial access complications
- vasospasm
- pediatric
- Hydrogel
- single practice
- Telestroke
- acute stroke
- stroke organization
- spinal pial fistula
- glue
- vertebro-vertebral fistula
- endovascular occlusion
- coiling
- flow reversal
- volumetry
- ASPECTS
- mRS
- biomarkers
