- Home
- About
- Editorial Team
- Browse
- Submissions
- Advertising
- ESMINT Website

The Journal of the Swiss Society of
Minimally Invasive Neurological Therapy
The Journal of the Swiss Society of
Minimally Invasive Neurological Therapy
What do lumbar puncture and jugular venoplasty say about a connection between chronic fatigue syndrome and idiopathic intracranial hypertension?
EJMINT Original Article, 2014: 1448000223 (24th November 2014)
Abstract
Keywords: cranial venous outflow obstruction, jugular venoplasty, chronic fatigue syndrome, idiopathic intracranial hypertension, lumbar puncture
Abbreviations
- IIH
- idiopathic intracranial hypertension
- CT
- computerised tomography
- CSF
- cerebrospinal fluid
- ICHD-2
- The International Classification of Headache Disorders: 2nd Edition
Introduction
Similarities between chronic fatigue syndrome and idiopathic intracranial hypertension (IIH) invite speculation that they may be related. Both are conditions of unknown aetiology. Both can develop without any clear precipitating factor at almost any age, in either sex and cause symptoms that can last for years [1-7]. Fatigue, though often submerged by more overt symptoms, is common in IIH. Headache is frequent in chronic fatigue syndrome. Impaired memory, poor concentration, depression, dizziness and joint pains occur in both [1,3,7-11]. Chronic fatigue syndrome presents no clinical signs and there are no confirmatory laboratory investigations. IIH presents only signs of raised intracranial pressure - mainly papilloedema - signs which may be absent [12-13].
The diagnosis of IIH requires only that intracranial pressure is abnormally high and that there is no known cause [6]. This definition recognises that that IIH may come in different forms. Headache may be absent; a patient presenting, for example, after papilloedema is found at fundoscopy performed in pursuit of visual symptoms [14]. Visual symptoms and papilloedema may be absent; this phenotype is named IIH without papilloedema, and such patients are only diagnosed after lumbar puncture, usually performed to evaluate headache [15-17].
Inevitably there will be cases of IIH, therefore, in which there is neither headache nor visual disturbance and in whom there are no signs of raised intracranial pressure. How might these cases be picked up? In other words, what would precipitate measurement of intracranial pressure in a patient who only suffered from the less remarked upon symptoms of IIH - impaired memory, poor concentration, depression, dizziness, joint pains and fatigue [7-11]: only a heightened awareness that these symptoms might be a product of abnormal intracranial pressure. In effect, since these symptoms form the basis of a diagnosis of chronic fatigue syndrome [1-3], only a heightened awareness that patients with chronic fatigue syndrome might have raised intracranial pressure.
In recognition of this problem we have been using lumbar puncture to screen selected patients with chronic fatigue to look for raised intracranial pressure [18-19] with results, in a first cohort of 20, that suggest that chronic fatigue syndrome represents a “forme fruste” of IIH. Thus, the mean intracranial pressure in this group was towards the upper limit of normal and the majority of patients responded positively when intracranial pressure was reduced by withdrawing cerebrospinal fluid [18-19].
Connecting chronic fatigue syndrome with IIH, of course, is to connect one condition of unknown aetiology with another. At first, this may not appear to be much of an advance; however, it does mean that speculation about the cause of one might be relevant to the other. It also means that treatments that bring clinical benefit to one might be useful in the other.
Regarding IIH, several aetiological mechanisms have been discussed, including obstruction to cranial venous outflow [20-23], an idea which has become the focus of attention in recent years with the development of venous sinus stenting as an alternative to other invasive treatments in difficult cases [24-29]. In regard to chronic fatigue, the same considerations might apply, including the prospect of treatment directed at cranial venous outflow if it can be shown that this is somehow impaired and that the impairment is of clinical importance.
This paper revisits the results of lumbar puncture in patients referred with chronic fatigue, a group now extended to 29 patients. It also describes the use of cerebral venography and jugular venoplasty to evaluate the clinical significance of focal narrowings in the internal jugular veins identified on CT venography.
Patients and methods
Since 2007, patients attending a specialist clinic at our institution, who fulfil the diagnostic criteria for chronic fatigue syndrome and in whom headache is a prominent symptom, have been offered CT venography and lumbar puncture looking for raised intracranial pressure. At the time of lumbar puncture, cerebrospinal fluid (CSF) is also withdrawn to trial the clinical effect of lowering intracranial pressure.
Patients diagnosed with unequivocal IIH as a result had their further management dictated mainly by uncontrolled symptoms (since none had papilloedema nor any other sign of raised intracranial pressure), this generally meaning catheter cerebral venography to establish the feasibility of venous sinus stenting [21-25]. Patients whose symptoms responded to CSF withdrawal but whose intracranial pressures were not high enough to satisfy the diagnostic criteria for IIH [30] have been managed in a similar way. In addition, any patient, regardless of their CSF pressure or response to CSF drainage, whose CT venogram showed focal narrowing of one or both internal jugular veins, was offered catheter venography and balloon angioplasty, attempting to establish its clinical significance.
Lumbar punctures were carried out under x-ray fluoroscopic guidance with the patient lying on their left side using a 22 gauge needle. Pressures were recorded using a manometer referenced to the point of needle insertion. CSF drainage was by gravity alone under medical supervision with the amount to be drained not specified beforehand and discontinued if there was onset of a new headache.
Catheter cerebral venography was carried out under local anaesthesia using a microcatheter supported by a 4 French diagnostic catheter from a femoral vein puncture. Pressure recordings, referenced to the mid axillary line, were transduced from the end of the microcatheter to a monitor.
For venoplasty, the 4 French catheter was exchanged for a 5 French guide catheter. This was used to support an angioplasty balloon catheter over a 0.014 guidewire generally sized to match the dimensions of the jugular vein on either side of the stenosis. Usually only one side was angioplastied, but occasionally both.
Results
Twenty-nine patients to date, 9 males and 20 females, with an average age of 37 years (range 16-70 years) have been referred for investigation of intracranial pressure. All satisfied the accepted criteria for chronic fatigue syndrome [1]. All had had symptoms for at least 6 months when first seen in clinic, (average 7 years; range 6 months to 30 years). No patient had papilloedema or any other sign of raised intracranial pressure.
Mean CSF pressure at lumbar puncture in the whole cohort of 29 patients was 19 cm H2O (range 12 - 41cm H2O). In 5, CSF pressures were high enough to diagnose IIH by ICHD-2 criteria [30].
Twenty-five patients responded positively to CSF withdrawal, including the 5 whom matched the criteria for IIH. In the other 20, CSF pressures were not high enough to allowed a diagnosis of IIH by ICHD-2 criteria, but there was still symptomatic improvement with CSF withdrawal.
Twenty-one patients were judged to have focal narrowing of the internal jugular veins close to the skull base on CT venography (Figures1-3). In 18 cases, this narrowing was bilateral. In 3 cases narrowing was unilateral.
 Figure 1CT venogram showing the jugular veins (arrows) on each side (a) just below the skull base, (b) adjacent to the lateral mass of the C1 vertebra and (c) at the C4 level. There is focal narrowing at the C1 level on both sides.
Figure 1CT venogram showing the jugular veins (arrows) on each side (a) just below the skull base, (b) adjacent to the lateral mass of the C1 vertebra and (c) at the C4 level. There is focal narrowing at the C1 level on both sides.
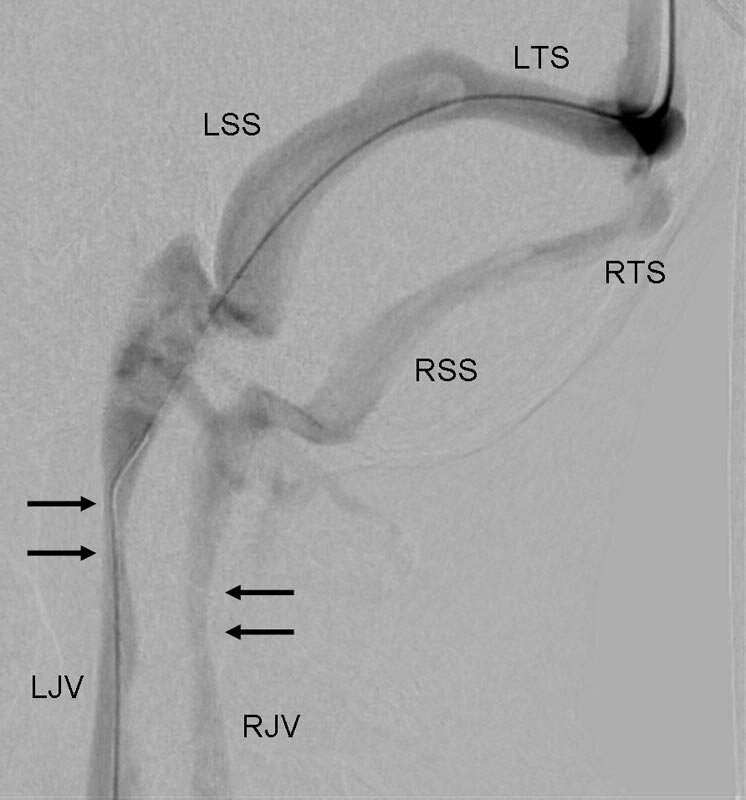 Figure 2Same patient. Tilted lateral view of the transverse and sigmoid sinuses and of the internal jugular veins at catheter venography. Radiographic contrast fills both sides after injection into the sagittal sinus. Narrowing seen on CT venography is evidenced by a subtle constriction of the internal jugular veins (arrows). (LTS = left transverse sinus; LSS = left sigmoid sinus; LJV = left jugular vein; RTS = right transverse sinus; RSS = right sigmoid sinus; RJV = right jugular vein)
Figure 2Same patient. Tilted lateral view of the transverse and sigmoid sinuses and of the internal jugular veins at catheter venography. Radiographic contrast fills both sides after injection into the sagittal sinus. Narrowing seen on CT venography is evidenced by a subtle constriction of the internal jugular veins (arrows). (LTS = left transverse sinus; LSS = left sigmoid sinus; LJV = left jugular vein; RTS = right transverse sinus; RSS = right sigmoid sinus; RJV = right jugular vein)
 Figure 3Same patient. (a) Lateral view showing angioplasty balloon inflated in the left internal jugular vein. (b) Same view, subtracted image, after withdrawal of the balloon showing no appreciable change in jugular morphology.
Figure 3Same patient. (a) Lateral view showing angioplasty balloon inflated in the left internal jugular vein. (b) Same view, subtracted image, after withdrawal of the balloon showing no appreciable change in jugular morphology.
Fourteen patients with jugular venous narrowing have had catheter venography and jugular venoplasty to date. These patients included 4 of the 5 with unequivocal IIH. The other 10 had lower CSF pressures, 7 who had responded to lumbar puncture and 3 whom had not. Pressure gradients across the jugular narrowings varied from 1 cm H2O to 8 cm H2O (mean 3 cm H2O). In 3 patients angioplasty was carried out on both sides at the same sitting. In the rest only one side was treated.
Most patients experienced local discomfort at the site of venoplasty, usually settling over a few minutes. No patient exhibited any appreciable change in angiographic appearances afterwards. All responded with an improvement in symptoms lasting from a few minutes to several weeks (Table 1). In most cases this improvement was noticed almost immediately. In 5 patients symptomatic improvement did not develop until a few days later. Most patients returned to their baseline state within a few days, but some were still experiencing a benefit more than a month later, though generally not as marked as in the early days. There were no adverse clinical events.
Discussion
Though not independent of work described in previous publications [18-19], the additional data presented here reinforce the observation that if headache is used as a catalyst to investigate intracranial pressure in patients with chronic fatigue syndrome, a sizable minority will be found to have IIH. At the same time, the data also reinforce the observation that a much larger proportion of these patients, whilst not having CSF pressures high enough to meet the criteria for IIH, will respond to CSF drainage in exactly the same way as those who do meet the criteria. Clearly, our patients were highly selected, the interventions were unblinded and there was no control group. Nevertheless, if chronic fatigue syndrome is being hypothesised as a variant form of IIH, these findings are supportive.
CT venography can be used as a non-invasive tool to give an idea of intracranial pressure, bilateral narrowing of the transverse sinuses strongly suggesting intracranial hypertension [31]. At the same time, however, if the examination is extended into the neck there is opportunity to examine the extracranial venous system in the knowledge that extracranial venous obstruction is a well recognised cause of raised intracranial pressure and, more specifically, that jugular venous obstruction at the C1 level has been implicated in cases of IIH [32]. If chronic fatigue syndrome is a variant form of IIH, there is no reason why extracranial venous obstruction may not be a factor here as well.
Looking particularly at the extracranial venous system in our patient group, we found focal narrowings of the jugular veins just below the skull base in the large majority. Moreover, in those who went on to have venoplasty, all responded with an improvement in symptoms. Again, our patients were highly selected; that is, they were selected on the basis of prominent headache at the discretion of the clinician running the clinic, which means that the results may not be applicable to the wider population with chronic fatigue. Moreover, as would be expected in a record of clinical practice, there was no control group to reduce bias or to eliminate the effect of placebo. Equally, there was no systematised recording of the clinical effects of venoplasty and any response, however brief, was taken as a positive (Table 1). Nevertheless, headache is common in chronic fatigue and with the response rate we recorded, these confounding effects would have to be very strong indeed for the results to have no clinical relevance.
Clearly, this is preliminary work and there are important caveats. Even so, the results of jugular venoplasty ask novel questions about the nature of chronic fatigue. Taken with the results of lumbar puncture [18-19], they invite speculation that chronic fatigue syndrome is a disorder of intracranial pressure, similar to, but less extreme, than IIH, in which cranial venous outflow obstruction is an important aetiological factor. All 14 of our patients who had venoplasty had a positive clinical response to the procedure, 11 of whom had already shown a positive response to CSF withdrawal. Venous outflow obstruction would provide an explanation for the clinical response to both interventions.
The notion that cranial venous outflow obstruction might play a part in the aetiology of IIH is not new and has been the subject of debate [20-23]. Patients with IIH have been investigated with catheter venography which has shown high pressures in the venous sinuses, usually upstream of stenoses in the transverse sinuses [20-21]. There is uncertainty over whether these stenoses represent primary venous obstruction or are a secondary phenomenon, that is, the result of compression of the venous sinuses by raised intracranial pressure [22-23]. However, regardless of the mechanism operating, dilating these stenoses with stents can give good palliation, testifying to their importance in the development of symptoms [24-29].
Jugular venous narrowing has not received much attention in IIH mainly because the pressure gradients observed across the transverse sinuses seem to dwarf anything measured outside the skull and it would seem counterintuitive to investigate small pressure gradients in the jugular veins when there are very large gradients elsewhere along cranial venous outflow [21]. In chronic fatigue syndrome, however, our experience has been that intracranial pressures are generally lower than in patients with unequivocal IIH and this striking dissimilarity between intracranial and extracranial pressure gradients is no longer evident. In these circumstances, therefore, if cranial venous outflow obstruction is going to be considered an issue, there is no reason why extracranial venous narrowings should not carry the same weight as intracranial.
That extracranial venous disease can cause raised intracranial pressure is well known, exemplified by the syndrome of superior vena cava obstruction. IIH is a more subtle disorder in terms of its physical signs but two cases have been described recently in which IIH appeared to have been caused by narrowing of the internal jugular veins between the styloid processes and lateral masses of the C1 vertebra [32]. The cases we describe in this report generally exhibited venous narrowings around the same level, including patients whose CSF pressures were sufficiently high to allow an unequivocal diagnosis of IIH. Interestingly, the four patients with unequivocal IIH who had venoplasty responded no differently from any of the others. If this is not a placebo effect, it suggests either that the clinical response to venoplasty is a non-specific indicator of some problem with intracranial pressure or that, despite the usual disparity between intracranial and extracranial pressure gradients in IIH, extracranial venous stenoses may be more important in IIH than previously recognised. Either way, they could be important in chronic fatigue.
Addendum following peer review
All the activity described in this paper was undertaken solely with the intention of benefiting each individual patient and with a reasonable chance of impacting on their clinical management and, therefore, did not require ethical approval according to guidance from the Royal College of Physicians of London. All patients described in this paper were severely compromised in their quality of life and had exhausted or refused all other treatment options. It was explained to them that we were offering a line of investigation based on our understanding of patients with IIH but that there was no precedent for it in the medical literature. They were counselled on separate occasions before and after CT venography, before and after lumbar puncture and before and after catheter venography and venoplasty.
In the context of a condition that offers no clue to its aetiology this paper is effectively an evaluation of a clinical practice designed to identify patients with chronic fatigue syndrome who might have a disorder of intracranial pressure. We have argued previously that this is a legitimate concern [18-19] and in this paper we argue that it follows that these patients could have a disorder of cranial venous outflow. Inevitably, this approach to a clinical problem leaves many questions unanswered. Inevitably, our own practice will have evolved in the 7-year period since the start of this initiative in response to what were finding. This both limits and strengthens the paper.
Regarding limitations, the value of the work is affected by bias in the selection of patients from clinic, the lack of specific criteria on what constitutes prominent headache, unspecified criteria on what constitutes a focal narrowing of the internal jugular veins, the lack of a control group and unblinded interpretation of data. This means we have little idea of the effect of placebo. Equally, we do not establish criteria for who should be investigated in this way and it is difficult to extrapolate the findings to the wider group of patients with chronic fatigue.
Regarding the strengths of the paper, however, the failure to specify what headache beyond “prominent” should precipitate a referral for lumbar puncture and the failure to specify criteria for what constitutes significant narrowing of the jugular veins would normally be considered a handicap, that is, likely to reduce the chance of obtaining a statistically significant result in a scientific study; yet, we were still able to show quite striking results. This suggests either that the placebo effect is very strong indeed or that we are looking at important clinical phenomena.
In summary, this paper is not an attempt to define the various parameters that would dictate the probability of IIH or venous outflow obstruction in patients with chronic fatigue, nor is it an attempt to establish the prevalence of these conditions in patients with chronic fatigue. It does, however, present a hypothesis amenable to testing and, thereby, a challenge to explore these issues further.
Conclusions
Accepting the caveats that accompany the interpretation of unblinded, uncontrolled data, the results of lumbar puncture and CSF withdrawal in our patient group lend support to the idea that chronic fatigue syndrome represents an incomplete form of IIH. Furthermore, the response of patients with chronic fatigue syndrome to jugular venoplasty suggests that cranial venous outflow obstruction may be an aetiological factor.
Acknowledgments
Prof Pickard is in receipt of an NIHR Senior Investigator Award.
Conflict of interest
We declare that we have no conflict of interest.
References
- Fukuda K, Straus SE, Hickie I et al.; The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group; Ann Intern Med. 1994; 121(12): 953-9.
- Wessely S, Chalder T, Hirsch S et al.; The prevalence and morbidity of chronic fatigue and chronic fatigue syndrome: a prospective primary care study; Am J Public Health. 1997; 87(9): 1449-55. [PubMed]
- Evengård B, Schacterle RS, Komaroff AL; Chronic fatigue syndrome: new insights and old ignorance; J Intern Med. 1999; 246(5): 455-69. [PubMed] [Full Text Sources]
- Wall M, George D; Idiopathic intracranial hypertension. A prospective study of 50 patients; Brain. 1991; 114: 155-80. [PubMed] [Full Text Sources]
- Sussman JD, Sarkies N, Pickard JD; Benign intracranial hypertension. Pseudotumour cerebri: idiopathic intracranial hypertension; Adv Tech Stand Neurosurg. 1998; 24: 261-305. [PubMed]
- Friedman DI, Jacobson DM; Diagnostic criteria for idiopathic intracranial hypertension; Neurology 2002; 59(10): 1492-5. [PubMed] [Full Text Sources]
- Binder DK, Horton JC, Lawton MT et al.; "Idiopathic intracranial hypertension"; Neurosurgery 2004; 54 (3): 538–51
- Kleinschmidt JJ, Digre KB, Hanover R; Idiopathic intracranial hypertension: relationship to depression, anxiety, and quality of life; Neurology. 2000; 54(2): 319-24. [PubMed] [Full Text Sources]
- May M, Emond A, Crawley E; Phenotypes of chronic fatigue syndrome in children and young people; Arch Dis Child. 2010; 95(4): 245-9.
- Round R, Keane JR; The minor symptoms of increased intracranial pressure: 101 patients with benign intracranial hypertension; Neurology 1988 Sep;38(9):1461-4. [PubMed]
- Johnston I, Owler B and Pickard J; The Pseudotumor Cerebri Syndrome: Pseudotumor Cerebri, Idiopathic Intracranial Hypertension, Benign Intracranial Hypertension and Related Conditions; Cambridge: Cambridge University Press 2007
- Marcelis J, Silberstein SD; Idiopathic intracranial hypertension without papilledema; Arch Neurol. 1991; 48(4): 392-9 [PubMed] [Full Text Sources]
- Digre KB, Nakamoto BK, Warner JE et al.; A comparison of idiopathic intracranial hypertension with and without papilledema; Headache 2009 Feb;49(2):185-93. [PubMed] [Full Text Sources]
- Lim M, Kurian M, Penn A et al.; Visual failure without headache in idiopathic intracranial hypertension; Arch Dis Child. 2005 Feb;90(2):206-10. [PubMed] [Full Text Sources]
- Mathew NT, Ravishankar K, Sanin LC; Coexistence of migraine and idiopathic intracranial hypertension without papilledema; Neurology 1996; 46(5): 1226-30. [PubMed]
- Bono F, Messina D, Giliberto C et al.; Bilateral transverse sinus stenosis predicts IIH without papilledema in patients with migraine; Neurology 2006; 67(3): 419-23 [PubMed] [Full Text Sources]
- Bono F, Messina D, Giliberto C et al.; Bilateral transverse sinus stenosis and idiopathic intracranial hypertension without papilledema in chronic tension-type headache; J Neurol. 2008; 255(6): 807-12. [PubMed] [Full Text Sources]
- Higgins N, Pickard J, Lever, A; Looking for Idiopathic Intracranial Hypertension in patients with Chronic Fatigue Syndrome; J Observational Pain Medicine 2013; 1(2): 28-35.
- Higgins N, Pickard J, Lever A; Lumbar puncture, chronic fatigue syndrome and idiopathic intracranial hypertension: a cross-sectional study; Journal of the Royal Society of Medicine Short Reports 2014; 4(12) 1–7. DOI: 10.1177/2042533313507920
- Karahalios DG, Rekate HL, Khayata MH et al.; Elevated intracranial venous pressure as a universal mechanism in pseudotumor cerebri of varying etiologies; Neurology 1996; 46(1): 198-202. [PubMed]
- King JO, Mitchell PJ, Thomson KR et al; Cerebral venography and manometry in idiopathic intracranial hypertension; Neurology 1995; 45(12): 224-8.
- King JO, Mitchell PJ, Thomson KR et al; Manometry combined with cervical puncture in idiopathic intracranial hypertension; Neurology 2002; 58: 26-30. [PubMed] [Full Text Sources]
- Silberstein SD, McKinstry RC 3rd; The death of idiopathic intracranial hypertension? Neurology 2003 May 13;60(9):1406-7.
- Higgins JN, Owler BK, Cousins C et al.; Venous sinus stenting for refractory benign intracranial hypertension; Lancet 2002; 359(9302): 228-30. [PubMed] [Full Text Sources]
- Higgins JN, Cousins C, Owler BK et al.; Idiopathic intracranial hypertension: 12 cases treated by venous sinus stenting; J Neurol Neurosurg Psychiatry 2003; 74(12): 1662-6. [PubMed] [Full Text Sources]
- Donnet A, Metellus P, Levrier O et al.; Endovascular treatment of idiopathic intracranial hypertension: clinical and radiologic outcome of 10 consecutive patients; Neurology 2008; 70(8): 641-7. [PubMed] [Full Text Sources]
- Bussière M, Falero R, Nicolle D et al.; Unilateral transverse sinus stenting of patients with idiopathic intracranial hypertension; Am J Neuroradiol. 2010; 31(4): 645-50. [PubMed] [Full Text Sources]
- Ahmed RM, Wilkinson M, Parker GD et al.; Transverse sinus stenting for idiopathic intracranial hypertension: a review of 52 patients and of model predictions; Am J Neuroradiol. 2011; 32(8): 1408-14. [PubMed] [Full Text Sources]
- Puffer RC, Mustafa W, Lanzino G; Venous sinus stenting for idiopathic intracranial hypertension: a review of the literature; J Neurointerv Surg. 2013 Sep;5(5):483-6. [PubMed] [Full Text Sources]
- The International Classification of Headache Disorders: 2nd edition. Cephalalgia 2004; 24(Suppl. 1): 9-160.
- Higgins JN, Tipper G, Varley M et al.; Transverse sinus stenoses in benign intracranial hypertension demonstrated on CT venography; Br J Neurosurg. 2005; 19(2): 137-40.
- Dashti SR1, Nakaji P, Hu YC et al.; Styloidogenic jugular venous compression syndrome: diagnosis and treatment: case report; Neurosurgery 2012 Mar;70(3):E795-9
Copyright © 2014 Swiss association of Minimally Invasive Neurological Therapy
Swiss association of Minimally Invasive Neurological Therapy Alerts
 latest news & articles
latest news & articles
Keywords
- intracranial aneurysms
- endovascular treatment
- flow diverter
- clopidogrel resistance
- training
- UEMS
- charter
- neuroradiology
- Interventional
- INR
- pharmacogenetics
- aneurysm
- pipeline embolisation device
- silk flow diversion device
- stents
- intracranial
- stroke
- interventional neuroradiology
- thrombectomy
- thrombolysis
- endovascular
- stroke treatment
- mechanical thrombectomy
- stent retriever
- magnetic resonance angiography
- intracranial aneurysm
- subarachnoid haemorrhage
- computed tomography
- angiography
- flow diversion
- cerebral
- delayed rupture
- Y stent
- cerebral aneurysm
- embolisation
- wide-neck aneurysm
- stent-assisted coiling
- anterior circulation aneurysm
- acute ischemic stroke
- randomised clinical trials
- carotid artery stenting
- high-risk
- complications
- flow disruption
- WEB
- tPA
- stent
- balloon-assisted
- stability
- sedation
- anesthesia
- transcarotid
- platelets
- haemorrhage
- thrombosis
- carotid stenting
- proximal balloon protection
- intracranial haemorrhage
- coils
- clipping
- acute stroke therapy
- ischaemic stroke
- MRI
- rtPA
- cranial venous outflow obstruction
- jugular venoplasty
- chronic fatigue syndrome
- idiopathic intracranial hypertension
- lumbar puncture
- cerebrovascular occlusion
- brain infarction - posterior circulation
- brain infarction – anterior circulation
- predictors
- femoral arterial access complications
- vasospasm
- pediatric
- Hydrogel
- single practice
- Telestroke
- acute stroke
- stroke organization
- spinal pial fistula
- glue
- vertebro-vertebral fistula
- endovascular occlusion
- coiling
- flow reversal
