- Home
- About
- Editorial Team
- Browse
- Submissions
- Advertising
- ESMINT Website

The Journal of the Swiss Society of
Minimally Invasive Neurological Therapy
The Journal of the Swiss Society of
Minimally Invasive Neurological Therapy
Pharmacogenomic approach to Clopidogrel resistance in patients with stent-assisted endovascular treatment of non-ruptured intracranial aneurysms
EJMINT Original Article, 2015: 1543000269 (22nd October 2015)
Abstract
Introduction
Antiplatelet drug resistance remains a clinical challenge both in cardiovascular as well as in neurovascular treatment. Considering the fact that clopidogrel premedication and dual antiplatelet treatment including clopidogrel after the procedure is, in spite of some new antithrombotic agents, still the gold standard for endovascular approach, clopidogrel resistance remains a clinical challenge [1-3] Results of several studies showing association of clopidogrel resistance with thromboembolic events during and after endovascular procedures emphasises the importance and need for detecting subjects with clinically relevant clopidogrel resistance [1-2].
Clopidogrel-induced platelet inhibition is patient-specific and prevalence of clopidogrel nonresponseveness in the population is between 4 % and 30 % (perhaps even up to 40 % in some studies) [1-2, 4]. Clopidogrel itself is a thienopyridine derivate, which inhibits platelet aggregation induced by adenosine diphosphate (ADP) [1, 4-5]. It is a prodrug, mediated mainly by cytochrome P-450 isoenzymes (CYP). Clopidogrel active metabolite binds irreversibly to the platelet ADP receptor P2Y, inhibiting platelet function during the whole platelet's life span. However, only 15 % of the prodrug is available for transformation to the active drug, while 85 % is deactivated by enzymes. Conversion of clopidogrel prodrug into its active metabolite requires several CYP450 enzymes [1-2, 5-6]. One of them, CYP2C19 enzyme, is the major determinant for clopidogrel metabolism in humans. CYP2C19 gene, on the other hand, is highly polymorphic and has more than 25 known variant alleles, CYP2C19*1 allele being the functional one. The most common CYP2C19 loss-of-function allele is 2*, having the frequency of approximately 15 % in Caucasians. One other polymorphism, CYP2C19*17 shows increased activity and therefore may increase bleeding risk in carriers. Apart from the CYP2C19 system, a form of P-glycoprotein system encoded by MDR1 gene is also important for clopidogrel bioavailability. Variance of MDR1 gene predicts absorption of clopidogrel and its transport activity affects oral bioavailability of clopidogrel. However, studies investigating this effect on clopidogrel resposeveness remain inconclusive [1-2, 4-6]. Furthermore, recent data reveal different extrinsic factors (e.g. life habits, body mass index and/or drugs) which may influence clopidogrel availability [7].
Clopidogrel resistance or non-responseveness seems to be an important factor for development of thrombotic complications in endovascular procedures [6, 8]. Many laboratory techniques have been developed in order to predict non-responders and prevent thrombotic complications during and after endovascular treatment [8-10]. Widely used and accepted methods are point-of-care antiplatelet function tests which are quick and cost-effective methods for evaluating clopidogrel response in patients. However, a major disadvantage of these tests is that their results do not always correlate with clinical findings,. The number of non-responders revealed by this method is still much higher than number of observed clinical complications [11-15], which highlights the need for more accurate ways of predicting and avoiding thrombotic complications.
This study aimed to compare CYP2C19 polymorphism and MDR1 variances with point-of-care aggregometry test results in clopidogrel premedicated patients with non-ruptured intracranial aneurysms who were scheduled for stent-assisted endovascular treatment. Such a prospective study has, to our knowledge, not been published to date.
Study design
We aimed to investigate possible correlations between genotype and phenotype for clopidogrel non-respondance with angiographic and clinical complication rate in patients with unruptured intracranial aneurysm treated with stent assisted coilling or stent alone in our institution. We designed a prospective study for our patient cohort with planned elective endovascular treatment during the 6 month period October 2014 - February 2015. Suitable patients for the study were otherwise healthy persons (with no significant comorbidity or permanent medical therapy, not heavy smokers defined as smoking <10 cigarettes/day, or having BMI more than 30), no more than 65 years of age with unruptured intracranial aneurysms and assumed need for stent assisted coilling during endovascular procedure. Informed consent was obtained from patients meeting study criteria. We took blood for genetic testing for CYP2C19 and MDR1 polymorphism before the interventon. All patients were premedicated for the endovascular intervention with oral dual antiagregation therapy with clopidogrel (either administered as 600 mg given 16 and 4 hours before the intervention, or consecutive doses of 75 mg per day for at least 5 days, the last dose being 4 hours before the intervention) plus aspirin (single dose of 100 mg 4 hours before the intervention). Three hours after intake of both medications, resistency was checked on a Multiplate (Roche) analyser, with ASPI test for aspirin and ADP test for clopidogrel.
The ASPI test uses the method of cyclooxygenase-dependent aggregation (using arachidonic acid) sensitive to aspirin and other inhibitors of platelet cyclooxygenase. The ADP test is used for the quantitative in vitro determination of platelet function following stimulation of the platelet adenosine diphosphate receptors, using the reagent intended for use in platelet aggregation testing with whole blood on the Multiplate analyser. Used tubes were standardised as well as the whole collection system; for all patients commercial hirudin blood collection tubes were used.
For both tests we used hirudin blood collection tubes, with 300 uL of blood; the test was performed after 3 min of incubation (measuring time 6 min). The analyser continuously recorded platelet aggregation, and the adhesion and aggregation of platelets were transformed into arbitrary aggregation units (AU) and plotted against time. Area under the aggregation curve (AUC) was used as primary parameter. Cut-off values of ADP test are established in hirudin blood samples. High thrombotic risk (non-responder cut-off value) represent values higher than 45 U (1 U being 10 AU*min), while high bleeding risk represents values lower than 15 U. Responders are therefore between values of 16 and 44 U (160 – 440 AU*min).
All patients were under general anesthaesia during the procedure. The procedure itself was performed under standard conditions, which included heparinisation at the begining of the procedure with 3000-5000 IU of heparin (70 IU / kg) immediately after the guiding cateter was inserted. Activated coagulation time was controlled and kept at 3-fold increase over its normal values during the whole procedure by one-hour regimen value checkings, and giving additional dosage of heparin (1000 IU) if needed. Final endovascular technique was chosen and applied by the best knowledge and experience of the interventional neuroradiologist on our team. All patients had control angiography 20 min after the procedure, after which they were, according to our routine procedures, monitored in our Neurological Intensive Care Unit. Initial neurological exam was done immediately after being woken from anesthaesia, and a control neurological exam 24 h after the treatment. After the procedure, all patients remained on dual antiplatelet therapy (75 mg of clopidogrel and 100 mg of aspirin daily for 3 months, according to our standard procedure.
For the purpose of our study, we only selected patients who showed no resistance to aspirin on ASPI test. In selected patients we analysed and compared their demographic data (age, sex), localisation of the aneurysm, used endovascular material (stent + coils, or only stent), results of genetic analysis (genetic polymorphism, variants), results of the ADP tests for clopidogrel, dosing regimen for clopidogrel and incidence of angiographic and/or clinical complications during the procedure, 24 h after the procedure and on follow up exam 3 months after the treatment (angiographic and clinical assessment). The primary aim of the study was to investigate correlation of genetic polymorphism in our patients with their aggregometry results but also ascertain the possible influence of those parameters on angiographic and clinical complications.
The statistical analysis was performed using the IBM SPSS software, version 20. Differences in the distribution of qualitative variables were determined with the χ2 test. For statistical analysis we used Pearson Chi-Square test. Due to the relatively small sample size, significance was calculated according to the Exact method.
Results
During our 6 month study, we treated 119 patients with 138 aneurysms. Sixty-three patients had unruptured intracranial aneurysms which met our basic criteria. We were able to analyse data from 37 patients (with 41 aneurysms) who met all of our study criteria and were treated between October 2014 – March 2015. Our study group comprised 12 (32 %) male and 25 (68 %) female patients, aged from 29 – 65 years (55 ± 7.6) (Figure 1). Patients' characteristics are presented in Table 1.
 Figure 1Male and female ratio in our patient group: 12 (32%) male and 25 (68%) female patients
Figure 1Male and female ratio in our patient group: 12 (32%) male and 25 (68%) female patients
Aneurysm localisation included: internal carotid artery (27 aneurysms), anterior communicating artery (4 aneurysms), middle cerebral artery (4 aneurysms), posterior communicating artery (1 aneurysm), posterior cerebral artery (1 aneurysm) and basilar artery (4 aneurysms) (Figure 2).
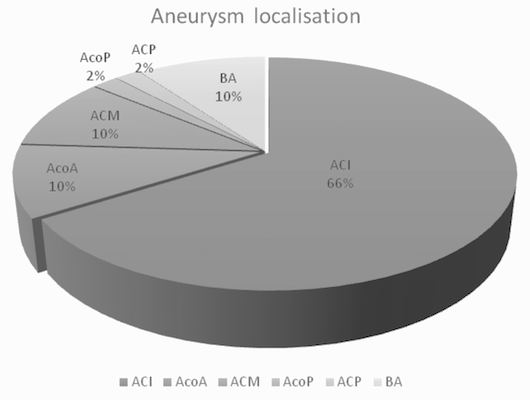 Figure 2Distribution of aneurysm localisation: 37 patients with altogether, 41 aneurysms. 4 patients (11%) had multiple aneurysms. ACI: 27 aneurysms, AcoA: 4 aneurysms, ACM: 4 aneurysms, AcoP: 1 aneurysm, ACP: 1 aneurysm, BA: 4 aneurysms.
Figure 2Distribution of aneurysm localisation: 37 patients with altogether, 41 aneurysms. 4 patients (11%) had multiple aneurysms. ACI: 27 aneurysms, AcoA: 4 aneurysms, ACM: 4 aneurysms, AcoP: 1 aneurysm, ACP: 1 aneurysm, BA: 4 aneurysms.
Four patients had multiple aneurysms.
Applied techniques and endovascular materials were flow diverters only in 4 patients, flow diverters and coils in 1 patient, stent only in 9 patients, coils only in 7 patients and stent and coils in 16 patients. The stents were Enerprise (J&J) in 17 patients, Neuroform (Stryker) in 8 patients and Silk (FD, Balt) in 5 patients. Applied techniques are presented in Figure 3.
 Figure 3Applied techniques for our patients FD (SILK, Balt): 4 patients, FD+C: 1 patient, S: 9 patients, C: 7 patients, S+C: 16 patients
Figure 3Applied techniques for our patients FD (SILK, Balt): 4 patients, FD+C: 1 patient, S: 9 patients, C: 7 patients, S+C: 16 patients
All patients were premedicated according to our protocol. Eighteen patients received a loading dose of 2 x 600 mg of clopidogrel and 19 patients received consequtive premedication during at least 5 days of 75 mg /day clopidogrel. All patients received 100 mg of aspirin 4 hours before the intervention. We performed pharmacogenetic testing for polymorphism of CYP2C19 in all selected patients before the intervention, and point-of-care testing for aspirin and clopidogrel resistance on Multiplate analyser 3 hours after the last dose of antiagregation therapy using ASPI and ADP tests. Aspirin non-responders were excluded from further analysis and treated with individual protocols (depending on test results for clopidogrel). Patient who were non-responders for clopidogrel (and included in the study) were carefully monitored and heparinised during the intervention and, after stent detachment, put on continuous antitrombotic prophylaxis with eptifibatide (2 ug/kg/min) during the next 24 h. In Figure 4 we present CYP2C19 polymorphism in our group of patients. Most patients (38 %) had 1*/1* allele, which is expected. We had a slightly greater proportion of patients with 1*/17* as well as with 2*/1* polymorphism (both 24 %) than it is known from literature. This might be the consequence of small number of subjects, but also a population characteristic. The proportion for other two polymorphisms (2*/17* 11% and 2*/2* 3 %) is expected. The patient with CYP2C19 2*/2* polymorphism, due to the rarity of this polymorphism, as well as due to increased risk for thrombotic complications, is presented separately (Table 3). This patient had a wide neck asymptomatic aneurysm on left ACI, for which the best treatment option was a flow diverter (SILK) stent placement. The patient was premedicated with clopidogrel for 7 days, and 100 mg of aspirin on procedure day; however, his aggregometry result marked him as a non-responder. Therefore, the patient was carefully monitored during the procedure and immediately after stent in-placement received a standard dose (infusion) of eptifibatide. In spite of the findings which put him in a high-risk patient group, the patient did not experience any early or late complications (Table 2).
 Figure 4Distribution of diverse genotypes for CYP2C19 polymorphism in our population We had 14 patients with 1*/1* genotype, 9 patients with 1*/17* genotype, 9 patients with 1*/2* genotype, 4 patients with 2*/17* genotype and 1 patient with 2*/2* genotype. In this chart we show a percentage of different genotypes in our population.
Figure 4Distribution of diverse genotypes for CYP2C19 polymorphism in our population We had 14 patients with 1*/1* genotype, 9 patients with 1*/17* genotype, 9 patients with 1*/2* genotype, 4 patients with 2*/17* genotype and 1 patient with 2*/2* genotype. In this chart we show a percentage of different genotypes in our population.
The patient complication group included 5 patients (13.5 %), all complications of a thrombotic nature (Table 3). However, just 2 patients (5.4 %) in our group had permanent complications. Two weeks after the procedure, one patient (2.7 %) died due to in-stent thrombosis which led to occlusion of the treated vessel (ACI) and a massive stroke. The other three patients had either no clinical complications – in spite of angiographic finding of thrombus formation (1 patient) - or their neurological impairment resolved almost entirely (mRs 0-1). Interestingly, 4 patients had CYP2C19 polymorphism of 1*/2*, and one had 1*/17*. Although the number is small, gene polymorphism distribution leads us to further analysis. Aggregometry results, on the other hand, were very different and just 1 patient with 1*/2* polymorphism had a non-responder value. According to aggregometry results, 3 patients were eligible to be described as hyper responders; however, genetic results showed the opposite.
Finally, we statistically analysed and correlated the CYP2C19 gene polymorphism with aggregometry results in our patients. Unsurprisingly, we did not find any correlation between gene polymorphism and results of aggregometry (Table 4). The next step was to correlate dosage regimen of clopidogrel with aggregometry results, which was also not clinically significant, indicating that the way of dosing is not influencing the aggregometry result (Table 5).
Finally, we analysed results of the variants of MDR1 transporter, and again, there was no correlation or clinical significance between those variants and aggregometry results (Table 6). However, none of the patients in Group 2 (low transport activity and longer bioavailability of drug), had non-responder aggregometry values, while in the group of patients with high MDR1 transport activity, 13 % were non-responders when disregarding other factors.
In spite of not reaching statistical significance, those results show some trend towards significancy of the MDR1 transport activity. The most intringuing result, however, was the only statistically significant finding: namely, the statistical significance between the genotype and complication rate. In our very small group of patients, we found statistically significant correlation between genetic polymorphism and complication rate, while in contrast we found no statistically significant correlation between aggregometry results and complication rate (Tables 7 and 8).
Discussion
The rate of thrombotic complications during endovascular, and especially neuroendovascular procedures, remains the highest of all complications. Yet, the idea of dual antithrombotic prevention therapy has been accepted as a standard protocol in most neuroendovascular centres and has a beneficial effect on reducing thrombotic complication rate. However, considering the relatively high percentage of noticed resistance (or non-responsiveness) for both routinely used drugs (aspirin and clopidogrel), recognising patients at risk and individualising the choice of antiplatelet therapy has become a priority. However, no guidelines recommend a routine method for measurement of platelet activity, especially when considering neuroendovascular procedures. Furthermore, most of the data about the resistance of antithrombotic drugs and consequent complications comes from the cardiovascular literature. Nevertheless, some studies of the incidence of thrombotic complications in neuroendovascular procedures describe a relationship between clopidogrel resistance and complications. Therefore, many neuroendovascular centres use methods to measure inhibition of platelet activity after ingestion of antithrombotic drugs.
The most widely accepted method is point-of-care testing of platelet inhibition. However, most studies do not confirm correlation between those test results and the clinically important complication rate, which may explain why such tests are not part of the guidelines for neuroendovascular procedures.
On the other hand, given the metabolism of clopidogrel, pharmacogenetic testing may give more precise data about responsiveness of individuals to this drug. There is some evidence that allelic variants of CYP2C19 gene are the most important factor influencing the bioavailability of this drug. This raises a critical question regarding the relationship between genotype (CYP2C19 polymorphism) and phenotype (aggregometry results obtained in clinical setting) in premedicated patients. Investigation of this correlation was the main aim of our study. Our results showed no statistically significant correlation between these two parameters. One possible explanation for this result may be that point-of–care tests are routinely performed at specified hours after drug ingestion (the peak concentration of available drug) and results can be influenced by some other drugs and comorbidities. Therefore, test results represent an actual state of platelet reactivity, which might vary over time. Given that endovascular procedures may last for several hours, and that patients receive their next antiplatelet drug dosage 24 h after their previous one, the continuous state of platelet activity is probably not reflected in this single aggregometry value. For more reliable predicting of platelet activity and eventually early and late procedure outcome, several measurements of platelet function in different time windows from drug ingestion might be more helpful. Also, aggregometry point-of-care methods do vary to some extent, and results differ slightly from the gold standard; namely, the light transmission aggregometry test.
What's more, the results between different point-of-care methods may slightly differ. In our patient group we tried to eliminate known extrinsic factors and measured platelet activity with the Multiplate point-of-care test, which is not always correlated with light transmission aggregometry. According to some recently published papers, clopidogrel resistance measured by three different methods (light transmission aggregometry, VerifyNow and Multiplate) was extremely high (36-51 %), but lowest with the Multiplate method. However, the complication rate was less than 10 %. Interestingly, complications occured more frequently in patients whose resistance was confirmed by all three methods. These findings confirm the variability of aggregometry methods, which may, at least partly, explain lack of correlation between pharmacogenetic findings and single values of platelet activity.
Finally, our group of patients, due to strict inclusion criteria, was very small, so increasing the number of subjects might also change the final statistical result.
We also analysed one other genetic factor: the transport system for clopidogrel, which is a MDR1 system. This system is not dependent on most known factors which influence clopidogrel activity, and the MDR1 transport system is individually tailored and has normal, high or low activity. Depending on the individual MDR1 transport system, bioavailability of clopidogrel might be longer or shorter. In our group of patients, we did not find any statistical correlation between MDR1 activity and aggregometry results, but we did notice a trend towards normal or hyper responder values in patients with longer bioavailability of clopidogrel, discounting the finding of CYP2C19 polymorphism. This might explain different values of aggregometry disregarding genetic base or clinical outcome. For example, patients with low MDR1 transport activity and longer bioavailability of drug, might have false non-resistance (or even hyper responder) values on aggregometry at the moment of testing, but after several hours, the amount of active drug due to slow or diminished metabolism of the clopidogrel prodrug (which should be the function of CYP2C19 system) may be too low to maintain adequate platelet inhibition. Such a scenario could at least partly explain complication occurrence several hours after the procedure, even if the point-of-care test did not show any alarming result. The same could apply to individuals with high MDR1 activity and shorter bioavailability of the drug, but with adequate CYP2C19 function, which enables normal or expected metabolism of the prodrug. This theory needs further investigation and a much larger cohort of patients.
Nonetheless, CYP2C19 polymorphism is a life-long, stable parameter in predicting clopidogrel bioactivity which in our small patient cohort correlated much better with angiographic and clinical complications then any other examined parameter. This might imply that CYP2C19 gene polymorphism, especially loss-of-function allele 2*, might have a role in pretreatment evaluation and medical prevention of thrombotic complications. Our results reflect the importance of genetic testing, and could lead to individual (pharmacogenomic) tailoring of antiplatelet therapy. Aggregometry results might be more important in indicating and confirming platelet activity in subgroups of patient with normal metabolic activity (CYP2C19 allele 1*), or in a subgroup of patients with increased metabolic activity (allele 17*) where it can be helpful in recognising patients with higher bleeding risk during pretreatment and early post-treatment phase. In patients with gene polymorphism on 2* allele, the idea of some alternative therapies or therapy protocols might be reconsidered. In this group of patients, aggregometry results could be important in showing current state of platelet activity, but probably is not sensitive enough in predicting possible complications or confirming avoidance of complications.
Study limitations
The most important and striking study limitation is the small number of patients and the small number in each patient group. Although we performed statistical analysis for each planned parameter, our study may have been underpowered to detect significant results. A need for a larger study group is obvious and represents, in our opinion, the biggest study limitation. Furthermore, we used Multiplate point-of-care test which might also have influenced our final results. According to the literature, light transmission aggregometry results correlate with thromboembolic complications more accurately than the VerifyNow and Multiplate point-of-care methods, and there are some suggestions that VerifyNow method correlates with light transmission aggregometry better than other point-of-care methods.
Another problem is the lack of precise neurological assessment, including neuropsychological testing, as well as lack of early and control MRI findings for each patient, which might disclose subclinical or fine neurological deficits and a larger group of patients with complications, which could influence conclusions. Finally, a longer follow-up, of at least 1 year for each patient, is recommended.
We plan to continue our study on a larger group of patients during the next 3 years using light transmission aggregometry in conjunction with VerifyNow method for aggregometry tests, and precise neurological as well as neuroimaging controls for all subjects in order to avoid the above limitations.
Conclusion
Our study provides new insight into the premedication approach for patients with intracranial non-ruptured aneurysms assigned to endovascular stent-assisted treatment. The most feared complications in such patients are thrombotic incidents which are routinely prevented with different regimens of antiaggregation therapy. Clopidogrel resistance may be one important problem in predicting antiaggregation effect in this group of patients. Point-of-care tests, measuring antiaggregation effect of antithrombotics, are routinely used for creating individually tailored antiaggregation therapy. However, many studies fail to show adequate correlation between aggregometry results and complications during and after the procedure. Our results show that pharmacogenetic testing might also be useful in individually tailored antiaggregation therapy. CYP2C19 polymorphism as well as transport MDR1 activity appear to be parameters which, if proven on larger number of patients, could be helpful in predicting possible complications and selecting therapeutic approaches in certain group of patients.
To our knowledge this is the first publication which compares results of genetic testing (polymorphism of CYP2C19 gene), aggregometry results and MDR1 transport activity for clopidogrel with clinical outcome in patients after endovascular treatment of non-ruptured intracranial aneurysms. However, further investigation on larger study groups are needed to confirm our results and perhaps develop new recommendations for the optimal diagnostic and therapeutic approach in these patients.
Conflict of interest
We declare that we have no conflict of interest.
References
- Scott SA, Sangkuhl K, Gardner EE, et al.; Clinical Pharmacogenetics Implementation Consortium Guidelines for Cytochrome P450-2C19 (CYP2C19) Genotype and Clopidogrel Therapy; Clin Pharmacol Ther. 2011;90. 328-332 [PubMed] [Full Text Sources]
- Vlachojannis GJ, Dimitropoulos G, Alexopoulos D; Clopidogrel Resistance: Current Aspects and Future Directions; Hallenic J Cardiol. 2011;52:236-245
- Unemura K, Furuta K, Kondo K; The common gene variants of CYP2C19 affect pharmacokinetics and pharmacodynamics in an active metabolite of clopidogrel in healthy subjects; J. Thromb Haemost. 2008;6:1439-1441.
- George J, Doney A, Palmer NC, Lang CC; Pharmacogenetics Testing: Implications for Cardiovascular Therapeutics with Clopidogrel and Warfarin; Cardiovascular Therapeutics. 2010; 28:135–142
- Fifi JT, Brockington C, Narang J, et al.; Clopidogrel Resistance Is Associated with Thromboembolic Complications in Patients Undergoing Neurovascular Stenting; AJNR Am J Neuroradiol. 2013;34:716-720 [PubMed] [Full Text Sources]
- Hulot JS, Bura A, Villard E, et al.; Cytochrome P4502Blood. 2006;108:2244-2247.
- Gurbel PA, Bliden KP, Logan DK, et al.; The Influence of Smoking Status on the Pharmacokinetics and Pharmacodynamics of Clopidogrel and Prasugrel; Journal of the American College of Cardiology 2013; Vol. 62, No. 6
- Kang HS, Kwon BJ, Kim JE, et al.; Preinterventional Clopidogrel Response Variability for Coil Embolisation of Intracranial Aneurysms: Clinical Implications; AJNR. 2010;31:1206-1210. [PubMed] [Full Text Sources]
- Breet NJ, van Werkum JW, Bouman HJ, et al.; Comparison of platelet function tests in predicting clinical outcome in patients undergoing coronary stent implantation; JAMA. 2010;303:754-762. [PubMed] [Full Text Sources]
- Simon T, Verstyft C, Mary-Krause M, et al.; Genetic determinations of response to clopidogrel and cardiovascular events; N. Engl. J. Med. 2007;357:2001-2015.
- Jo KI, Yeon JY, Kim KH et al.; Predictors of thromboembolism during coil embolization in patients with unruptured intracranial aneurysm; Acta Neurochir (Wien). 2013;155:1101-1106.
- Kim B, Kim K, Jeon P, et al.; Thromboembolic Complications in Patients with Clopidogrel Resistance after Coil Embolization for Unruptured Intracranial Aneurysms; AJNR. 2014;39:1-7
- Altay T, Kang HI, Woo HH, et al.; Thromboembolic events associated with endovascular treatment of cerebral aneurysms; J. Neurointerv Surg. 2011;3:147-50. [PubMed] [Full Text Sources]
- Prabhakaran S, Wells KR, Lee VH, et al.; Prevalence and Risk Factors for Aspirin and Clopidogrel Resistance in Cerebrovascular stenting; AJNR. Am J Neuroradiol.; 29:281– 85
- Flechtenmacher N., Kammerer F., Dittmer R, et al.; Clopidogrel Resistance in Neurovascular Stenting: Correlations between light Transmission Aggregometry, VerifyNow adn the Multiplate; AJNR. AM J Neuroradiol. 2015; Aug 13
Copyright © 2015 Swiss association of Minimally Invasive Neurological Therapy
Swiss association of Minimally Invasive Neurological Therapy Alerts
 latest news & articles
latest news & articles
Keywords
- intracranial aneurysms
- endovascular treatment
- flow diverter
- clopidogrel resistance
- training
- UEMS
- charter
- neuroradiology
- Interventional
- INR
- pharmacogenetics
- aneurysm
- pipeline embolisation device
- silk flow diversion device
- stents
- intracranial
- stroke
- interventional neuroradiology
- thrombectomy
- thrombolysis
- endovascular
- stroke treatment
- mechanical thrombectomy
- stent retriever
- magnetic resonance angiography
- intracranial aneurysm
- subarachnoid haemorrhage
- computed tomography
- angiography
- flow diversion
- cerebral
- delayed rupture
- Y stent
- cerebral aneurysm
- embolisation
- wide-neck aneurysm
- stent-assisted coiling
- anterior circulation aneurysm
- acute ischemic stroke
- randomised clinical trials
- carotid artery stenting
- high-risk
- complications
- flow disruption
- WEB
- tPA
- stent
- balloon-assisted
- stability
- sedation
- anesthesia
- transcarotid
- platelets
- haemorrhage
- thrombosis
- carotid stenting
- proximal balloon protection
- intracranial haemorrhage
- coils
- clipping
- acute stroke therapy
- ischaemic stroke
- MRI
- rtPA
- cranial venous outflow obstruction
- jugular venoplasty
- chronic fatigue syndrome
- idiopathic intracranial hypertension
- lumbar puncture
- cerebrovascular occlusion
- brain infarction - posterior circulation
- brain infarction – anterior circulation
- predictors
- femoral arterial access complications
- vasospasm
- pediatric
- Hydrogel
- single practice
- Telestroke
- acute stroke
- stroke organization
- spinal pial fistula
- glue
- vertebro-vertebral fistula
- endovascular occlusion
- coiling
- flow reversal
